Abstract
Introduction: The prognosis of patients diagnosed with blast crisis (BC) chronic myeloid leukemia (CML) is dismal. Allogeneic stem cell transplantation (alloSCT) represents the only curative treatment option. In the current tyrosine kinase inhibitor (TKI) era, however, data on transplant outcomes in patients with BC CML, particularly those with active BC at transplant, are scarce. We hereby report on a multicentre, EBMT-registry based retrospective study of adult patients allografted for BC CML focusing on patients with active disease at transplant and pre-transplant prognostic factors.
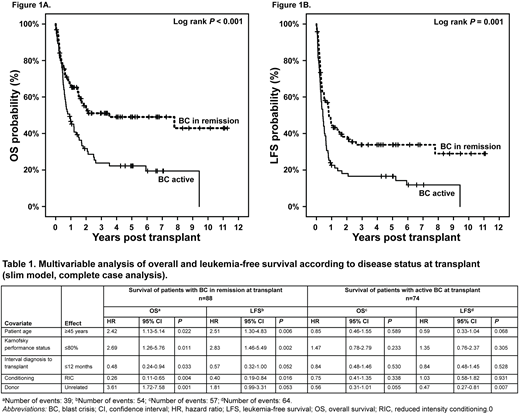
Patients and methods: Patients with BC CML at transplant (i.e. prior to the start of the conditioning) who underwent alloSCT after the year 2004 within the EBMT database were identified. Next, transplant centers were asked to report the exact disease status at transplant (including blood count, blast count in peripheral blood and bone marrow, achievement and type of remission with corresponding assessment dates, and the reason to proceed with alloSCT in BC CML). A total of 170 patients allografted for BC CML between 2004 and 2016 had complete data for analysis. Overall survival (OS) and leukemia-free survival (LFS) were calculated from date of alloSCT to the appropriate endpoint. For multivariable analysis of predictors of OS and LFS, Cox proportional hazard regression models were performed. Confounding prognostic factors (full models) were: age, disease status prior to alloSCT, Karnofsky performance status (KPS) prior to transplant, interval from diagnosis to transplant, year of transplant, stem cell source, conditioning intensity, donor type, and donor/recipient sex match. All patients provided informed consent for data collection and analysis.
Results: Median age at alloSCT was 45 years (range [r], 18-75). Median time from diagnosis to alloSCT was 13.9 months (r, 1.6-367.4). Median follow-up time was 54.7 months (r, 0.1-135.2). Stem cell source was peripheral blood, bone marrow and cord blood in 145 (85%), 18 (11%) and 7 (4%) patients, respectively. Donor types were: unrelated (UD), matched related, and mismatched related in 91 (54%), 64 (38%), and 15 (9%) patients, respectively. Conditioning was myeloablative in 108 (64%) of patients. KPS at alloSCT was ≤80% in 31% of patients. Information on BCR-ABL mutations was available for 41 patients; T315I was present in 28 patients. After thorough analysis of disease parameters, a total of 95 patients had any kind of remission of BC CML (including secondary chronic phase) prior to transplant (termed BC in remission); 75 patients had active BC CML prior to transplant (termed BC active). Main reason for proceeding with alloSCT despite active disease was resistance/refractoriness towards TKI in combination with polychemotherapy. Extramedullary disease was documented in 4 patients. In uni- and multivariable analyses of the entire cohort, besides low KPS, only disease status prior to transplant was significantly associated with shorter OS and LFS (for BC active: HR 2.00, 95%CI 1.35-2.96, p=0.001 and HR 1.80 95%CI 1.27-2.57, p=0.001, respectively). Accordingly, for patients allografted for active BC estimated 3-year OS and LFS was rather short (23.8% 95%CI 13.6-34.0 and 11.6% 95%CI 3.0-20.2, respectively) and significantly lower as compared to patients allografted for BC in remission (3-year OS and LFS: 51.1% 95%CI 40.5-61.7 and 33.8% 95% CI 23.6-44.0, respectively) (Figure 1A and B). Consequently, prognostic factors for survival were analyzed separately according to disease status at alloSCT (slim models, Table 1). For patients with BC in remission at transplant advanced age, lower KPS, shorter interval from diagnosis to transplant, myeloablative conditioning, and UD transplant were risk factors for inferior survival, whereas in patients allografted for active BC, only UD transplant was associated with prolonged LFS and with a trend towards improved OS (Table 1).
Conclusion: Survival of BC CML patients after alloSCT in the TKI era remains poor unless disease remission could be achieved. In patients who achieve remission prior to alloSCT, conventional prognostic indicators remain the determinants of transplant outcomes. In patients with active BC CML, UD transplantation appears to be associated with a survival advantage in our study.
Finke:Neovii: Consultancy, Honoraria, Other: travel grants, Research Funding; Medac: Consultancy, Honoraria, Other: travel grants, Research Funding; Riemser: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Other: travel grants, Research Funding. Tischer:Jazz Pharmaceuticals: Other: Jazz Advisory Board. Mayer:Eisai: Research Funding; Roche: Research Funding; Affimed: Research Funding; Novartis: Research Funding; Johnson & Johnson: Research Funding. Byrne:Novartis: Consultancy, Speakers Bureau; BMS: Consultancy, Speakers Bureau. Ganser:Novartis: Membership on an entity's Board of Directors or advisory committees. Chalandon:Roche: Membership on an entity's Board of Directors or advisory committees, Other: Travel costs.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal